Public health is referred to as a social science. Social Sciences are the fields that study how people live, work, learn, and interact. When you think about public health as a social science, it becomes clear why social factors shape both individual and population-level health.
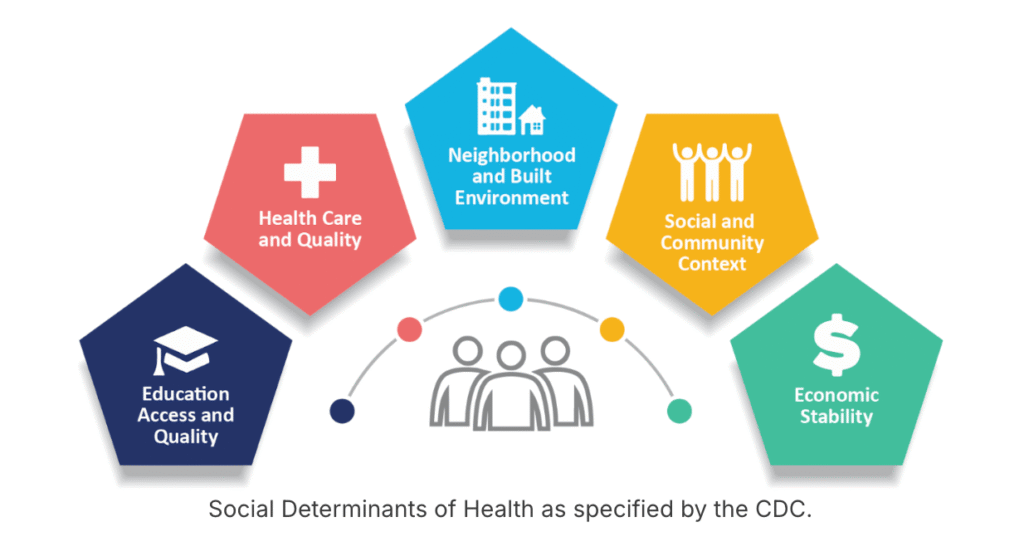
These social factors are referred to as social determinants of health (SDH).
Social determinants of health are defined by the World Health Organization as “the conditions in which people are born, grow, work, live, and age, and the wider set of forces and systems shaping daily life.”
These forces and systems include everything from economic policy and political systems to social norms and community resources.
Social determinants of health do not predict health outcomes. They influence probability. Individuals can thrive despite difficult environments, and others may struggle even with strong social advantages.
You can think about SDH as influencers that have powerful, wide-reaching effects. They don’t guarantee an outcome, but they shape the playing field.
Why Social Determinants Matter for Public Health Programming
Public health programming is most effective when it considers the social conditions that shape behavior and opportunity (we talked about how behavior theories can help shape public health programs last month!). SDH matter for several reasons:
1. Changing environments can be more effective than changing individual behavior
Policies like smoke-free public spaces reduced exposure to tobacco far more efficiently than convincing millions of people to quit, one at a time.
2. Unhealthy behaviors are often reinforced by the environments people live in
If someone lives in a neighborhood without grocery stores, safe parks, or reliable transportation, telling them to “just make a healthy choice” isn’t realistic.
3. Social Determinants of Health shift blame away from individuals
Many factors that shape health are outside someone’s control. When we assume a person is entirely responsible for their own health outcomes, it can lead us to judge who “deserves” care.
Blame also creates shame, and shame rarely motivates healthy change. Instead, it often makes things worse by reinforcing the very behaviors we hope to address. Public health works best when we focus on the conditions people live in, not on blaming individuals for circumstances they didn’t choose.
Understanding the Health Gradient
One of the most consistent phenomena in public health is the health gradient.
People with higher socioeconomic status (SES) tend to have better health, and those with lower SES tend to have poorer health at every step of the gradient.
SES is measured through:
- Income: wages, unemployment benefits, interest on investments
- Wealth: savings, retirement, assets
- Education: years completed and degrees earned
- Occupation: the social prestige associated with your job
In practice, this means health is shaped by:
- Stable jobs that offer insurance
- Ability to save for emergencies
- Lower chronic stress
- Access to strong social networks
- Living in safe neighborhoods with green space and affordable food options
Improving SES, even slightly, can improve the health of a population. Policies like increasing minimum wage, expanding job training, or creating affordable housing all move communities towards better health outcomes.
Other Key Determinants: Where We Live & Who We’re Connected To
Neighborhood & Built Environment
Where someone lives influences their access to:
- Nutritious food
- Walkable streets
- Green spaces
- Safe environments
- Mental respite from chronic stress and threat
These factors shape everything from diet and exercise to long-term cardiovascular and metabolic health.
Social & Community Context
Connection matters. Knowing you have support reduces stress. Feeling socially isolated, like many of us experienced during the pandemic, increases risk for depression, anxiety, and reduced healthy behaviors.
What This Means for Improving Public Health
When we understand the role of social determinants, we can design programs that:
- Address root causes, not just symptoms
- Create environments that make healthier choices possible
- Reduce blame and shame
- Support long-term, equitable change
Public health programming isn’t just about information, it’s about context. When we strengthen the social conditions that support health, we strengthen entire communities.
At CHIRP, we’re committed to helping community-based organizations navigate this complexity. Our goal is to make evidence-based public health more accessible by listening to community organizations and building programs based on the people that they serve.
Because when communities have the support, tools, and conditions they need to thrive, everyone benefits.




Pingback: What Is Health Equity? – Community Health Innovation & Resource Project